Following is the full transcript of the February 10th, 2020 Hudson event titled Containing the Coronavirus: Challenges to Thwarting the Outbreak
LEWIS LIBBY: Hello, everyone. Thank you. The Hudson Institute and the Bipartisan Commission on Biodefense would like to welcome you today to this session on the coronavirus. I am instructed to advise you that we will take questions during the session that will be used at the end, and you can send them in by tweet to @HudsonInstitute or by email to events@hudson.org. And that instruction will appear on the board during this session. We meet today at the intersection of rapidly advancing medical and geopolitical challenges. Medical concerns grow in the deepening shadow of illness, quarantine and, reportedly, hundreds of deaths in China. The stifled cry of a Wuhan doctor, dead of the virus at age 34, symbolizes the second challenge. His early warning about a spreading SARS-like virus was harshly sentenced by Chinese authorities. Back then, China downplayed the severity of the threat. Weeks later, China declared an emergency. In the West, many continue to question the Chinese statistics. In China, doubts about authorities advance in the wake of Hong Kong demonstrations and weaker detentions. Beneath the surface, beneath these statistics that mark these intertwined challenges, lurk human tragedies of a kind evoked by Camus and Solzhenitsyn, by Ibsen and Kessler.
Today's panel features some of the finest experts from both Hudson and the Bipartisan Commission. My name is Scooter Libby, and I'm lucky enough to play a small part in both of these institutions. Both rely on wide-ranging research to advance public debate and sound policies. Both institutions also benefit from terrific leadership - Hudson under Chairman Sarah Stern and President Weinstein and the Commission under its bipartisan co-chairs, Senator Joe Lieberman and former Pennsylvania governor and first Secretary of Homeland Security Tom Ridge. Today it is my high privilege and distinct honor, as that occasional phrase goes, to introduce our moderator, Senator Lieberman. Senator Lieberman is no stranger to homeland defense, national security or bipartisanship. Over his 24 years in the Senate, he was a powerful voice on the Senate Armed Services Committee, and he held important chairs, including on homeland security and governmental affairs. He also formed strong bipartisan partnerships with other Senate legends, including the late Senator John McCain and Senator Lindsey Graham. In 2000, Senator Lieberman was universally applauded as the Democratic nominee for vice president. Many still cite his vice presidential debate as a model of what such events should be. That debate was the first time that I got to study the senator close up, although he might say I was looking through the wrong end of the telescope.
(LAUGHTER)
LIBBY: Through either end, I saw then - and I still see - a patriotic, charismatic, compassionate and insightful man with strong friendships and many accomplishments across diverse fields. Currently, the senator is a partner in the well-regarded law firm of Kasowitz Benson in New York, helping to address our nation's critical shortage in talented lawyers.
(LAUGHTER)
LIBBY: Most relevant for today, Chairman Lieberman's Bipartisan Commission has produced multiple high-quality reports focused on natural and not-so-natural biological threats. Over the past five years, the Commission has advanced over 30 recommendations, over 20 of which have been either enacted or adopted as policies. Some of these recommendations, as you will hear, bear directly on today's topic. Finally and notably, the Commission has remained bipartisan - or rather tripartisan - in the highest sense of those terms - that is, not merely calculated political compromise but members of different parties with different backgrounds and viewpoints working together to get better results for our country. Please join me in welcoming Senator Lieberman.
(APPLAUSE)
JOE LIEBERMAN: Thanks very much, Scooter, for that really generous introduction and predictably literate, as you are. It's been a pleasure to get to know you after that little skirmish in 2000 ended, and we've been on the same side since. Also, thanks, through you, to the Hudson Institute for having, from the beginning, been both a host and a sponsor for our Bipartisan Commission on Biodefense. So let me give you just a real brief history about the commission. It's the inspiration of a man named Bob Kadlec, who has worked in the area of biodefense for some period of time in various administrations - actually is back now in this administration, working on that and other matters of public health. But Bob felt that our biodefenses were not up to the challenge. And by biodefenses, I mean defenses against both man-made biological threats - terrorism, bioterrorism - and naturally occurring biological threats such as infectious disease epidemics or pandemics, such as the one we are unfortunately experiencing now.
So Bob's idea for this was that we create a bipartisan commission to work on better preparing or urging the government to be better prepared for each of these potential biological attacks on the security of the American people. And it resulted in a six-person commission, which I'm honored to be co-chairing with former first Secretary of Homeland Security Tom Ridge, former Senate Majority Leader Tom Daschle, former secretary in the Cabinet, now a member of Congress, Donna Shalala, who left when she was elected to Congress to be replaced by Lisa Monaco, who, as far as I know, has not declared for Congress - yet was homeland security adviser in the Obama administration, Jim Greenwood, a former member of Congress, and Ken Weinstein, who was a - as a lawyer, has been an assistant U.S. attorney and was a homeland security adviser in the Bush 43 administration. So it's a wonderful group. Staff - excellent staff headed by Dr. Asha George. And I'm proud of what we've been able to do. We have - since we started in 2014, I learned a lot. And I will - some of the big things that I've learned are directly related to the current coronavirus pandemic.
One is the extent - well, the first is that though I was focused on bioterrorist acts the danger they represented to the American people - and they still do - that the potentially much more significant threats were naturally occurring infectious disease pandemics. Part of that we see from history. The influenza epidemic - pandemic - of 1918 killed over 50 million people worldwide. And more recently, we've dealt with MERS and SARS and Ebola and Zika. So this is - these are really serious. And the potential for them to occur is greater because of the greater extent to which we're traveling or involved in commerce every day with one another than certainly, was the case in 1918 when the flu epidemic occurred. The second - and after I'm done, the first speaker will deal with this - is a word that I use, let alone something substantive I learned, which is zoonotic, that most infectious diseases we're dealing with are zoonotic in the sense that they are transmitted to humans by various animal species. And how we deal with that is a really important question. We put out a report that's good or was good enough to mention in 2015. It had over 30 recommendations in it.
A key to the whole approach, I think was that there is no substitute in this area, as in so many others, for prevention, for preventive action. To me, one of the top conclusions, thematically, that I drew and have continued to draw from our work is that once an infectious disease epidemic starts, it's already, in one sense, too late - that the effort is focused on containing it. But if you start to scamper around, as we're doing right now to find treatments or vaccines, it's just about impossible to do that quickly. So then you do what we're doing now, which is to try to contain the spread of the disease. Of the 33 recommendations that we made, I think some of the most important dealt with organization of the U.S. government effort in this regard. One was to localize leadership - we recommended the vice president's office, but it's really important that somebody within the White House oversee all this - and that there be a strategy, which there was not. We recommended a national biodefense strategy. The - when the report came out, the Obama administration members of Congress supported it. But it wasn't until 2018, under President Trump, that the National Biodefense Strategy was actually issued. It's a good document. We're concerned in our commission that implementation of it has slowed a bit more than it should be, but all of this is now brought right to the center of our concerns and the public's concern, as well, with the novel coronavirus that we're dealing with now.
The numbers change every day, but they're really quite stunning and worrying. There have been a total of 40,171 people infected by the coronavirus, 908 deaths. Yesterday, just 97 deaths and 3,062 new cases. Almost all of these are in China. And I think we have to approach this as something that's happened in China now, but that could happen in the U.S. or anywhere else in the country - in the world. And I hope and am now pleased to see that there is an effort, not only through the World Health Organization, but through the United States government, to help our fellow citizens in China who are now at the - are now the targets, are immediately under risk from this coronavirus infectious disease, to help them in every way we can to contain it and to treat it and to, if it's possible now, to stop it. The administration has appointed a committee - the Trump administration - headed by Secretary Azar. It's an important thing to do. It's, in one sense, under the aegis - are involving the National Security Council. That's important because it makes the point that this spread of this disease is, in fact, a national security threat. It's - yes, it's a public health problem, but it is a national security threat. If we had our druthers based on our report, that committee that Secretary Azar heads would have already been appointed years ago and would be permanent and ready to spring into action with a crisis such as that presented now by novel coronavirus.
Secondly, we're very grateful to the CDC for having come up with a diagnostics test. That is, how do you find out if people showing symptoms, which in this case, are quite common, of actually having coronavirus? And the diagnostic kits have now been circulated within the last week by the Centers for Disease Control to states and localities, other governmental entities around the country. They're being shared around the world. NIH itself is working to produce a vaccine for a novel coronavirus, but that's not going to happen overnight. And we will talk about how that can happen. And again, going to the question of prevention and readiness, this crisis challenges us to invest in the development or the search for a broad spectrum of vaccine or antiviral, one that works against an entire class of pathogens like the coronavirus. There's also, in a much less complicated way, a real shortage of supplies to deal with a crisis like this. In addition to medical countermeasures, we've got to remember the need for essential medical supplies - basic stuff. There's no point, for example, in developing vaccines that need to be injected if we don't have enough needles. There's no point in telling hospitals and other health care deliverers to provide supportive care if we don't have supplies like saline. There's no point in urging everyone to take great care and protecting themselves if we don't have enough masks and gloves to go around. In fact, one expert we had appear before our commission a while back said that the world has only about a two-day surge capacity for these basic medical supplies; that is, items ordered and already manufactured, but have not reached their destination.
Just two days in the world, including, particularly, our friends in China, are dealing with this need and an urgent basis right now. Final word, the government's response - our government's response will only be as strong as available funds allow it to be. For a long time, unfortunately, Congress declined to provide funding for an entity it created, the Public Health Emergency Fund. Recently, it established a separate fund at the CDC and put in more than $100 million to combat infectious disease outbreaks. But today - as of today, just a little more than a month since our country began responding to the coronavirus, that rapid-response fund is totally depleted. And the CDC is having to take money away from other programs to keep funding novel coronavirus efforts. So it's clear that emergency supplemental funding is going to be necessary. I hope the administration will ask Congress for it quickly. And, needless to say, I hope and trust that Congress will respond. But again, there's no substitute for investments in preparedness for the next response. And when it comes to some of the real big investment items, like developing broad-spectrum antiviral vaccines or treatments, it's really a worldwide concern and ought to be - our funds ought to be pooled with funds from other countries around the world to see if we can combine our intelligence, our technology and our shared need as citizens of the same planet to be better ready for the next infectious disease epidemic when it breaks out.
We're very fortunate today - and the Bipartisan Commission on Biodefense is really proud to be co-sponsoring this event with the Hudson Institute to have brought together a wonderful group of experts. We're here to learn. And we're here to - hoping that we will learn some things that will help our commission and perhaps those of you who are here in the room and those watching on the livestreaming, to take action, to respond to the current threat and to prepare us to better respond to future threats. It is my great honor to begin by introducing Dr. Billy Karesh who is a member of our commission, one of the ex-officio members - we find a very clever way to keep the commission small but increase the expertise available to us. Billy and Scooter are both ex-officio members. Dr. Karesh is the executive vice president for the EcoHealth Alliance and brings a background as a veterinarian and will talk to us particularly about the zoonotic effect on this crisis. Dr. Karesh, it's all yours. You can speak from there or here, whatever you like.
KARESH: So welcome, everyone. It doesn't seem like it's been five years...
LIEBERMAN: It doesn't.
KARESH: ...Until you mentioned that. My, how time flies. And we've had some great outbreaks since then, haven't we?
(LAUGHTER)
LIEBERMAN: Yes. Yeah. I wanted to say that - just so people don't think this experience aged you - that, when I met you five years ago, you did not have any hair.
(LAUGHTER)
KARESH: That's right.
LIEBERMAN: So it's not the membership on this commission (laughter).
KARESH: This is very true. So once again, good afternoon. It's a pleasure to be here. Thanks for inviting me, Mr. Libby. I'm going to start out with a little video. And I think we're going to go in somewhat of a chronological order. So I want to take us back to why this outbreak's occurring and why similar outbreaks do occur. And we - before you cue up that video, the Hudson Institute asked me to specifically tell you there's a warning. You may see some things in this video that are unpleasant or uncomfortable. So if that is the case, you might want to close your eyes or shield your eyes. I'll narrate it for you. And also, it's adult content only.
LIEBERMAN: Right.
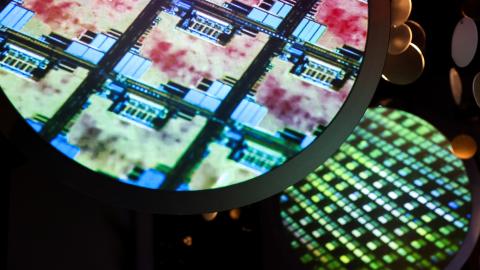
KARESH: And then, also, that I shot this video myself, so I do have the rights to it. And it was not taken in China. It was actually taken in Indonesia. So what I want to show you this is because this is not specifically a China issue. So much of the world gets their food on a daily basis from the systems that I'm going to show you. In fact, tens and tens and tens of millions of people are getting access - in contact with live animals and particularly wildlife in markets like the one I'm going to show you. Now, we've edited this down to just 30 seconds. I think the first time I showed it is while you were eating lunch.
(LAUGHTER)
KARESH: Apparently, that didn't go over so well. We've kind of trimmed this down for a cleaner section. You're not going to see the early part, where there's live dogs being killed and chopped up for food. You're going to miss out on the chickens there, some of the pigs. We're still going to give you a little flavor about what goes on in this market. So if you cue the video clip, those are actually bats for sale. At this one little market, they told me they were selling about 6,000 a week. And this market - of course, there's dozens of these markets in the neighboring area and one little, tiny place on one little island. And I think we just zipped by the rodents that were for sale. So those were rats for sale. And then this is fresh meat. I think this is pork, and somebody is chopping that up. Looks like they're still chopping up the bats. So you can see this mixing of blood and material, respiratory pathogens. They're all coming to the market. People are walking around in flip-flops. No one's wearing gloves. The consumers - the customers are handling it with their bare hands. The vendors are handling it with their bare hands. They touch their face. They bring in more live animals. That spreads more virus, bacterial pathogens. And the scale of this - as I said, there's thousands of these markets just in Asia alone. And we see it in Latin America and Africa, too. So we have thousands of markets on a daily basis with thousands of people. Now we're talking about millions of people exposed on a daily basis. So - and we seem to be surprised that there's emergence of a virus that goes from animals to people.
Well, I always say that the only thing surprising about this is that we are surprised by it. Everybody says it's - nothing we can do about it. And I disagree with that. For one thing is, if you look in those markets - and I was just in some in Cambodia recently - the only people in the markets are - the customers and the vendors are old people like me and then 5- and 6- and 7-year-old children whose grandparents are taking care of them because they're not in school. But that whole big demographic in the middle - average age in Asia is probably 20, 25 years old - they're not that interested in eating bats and this kind of food. They'd much rather go to Pizza Hut. I mean, if you asked your 18- or 20-year-old child, would you like to drink snake blood or would you like a hamburger from McDonald's? I think most of them will say, a burger from McDonald's. So I think there's an opportunity for this social behavior change, especially with social media that's rapidly growing in these parts of the world, that we can shift away from that. The other thing is modernizing the food safety programs. And that's really about refrigeration, cold storage, food safety. I think - I mean, it's not a joke, but I think this will eventually die away if it doesn't kill us while we're doing it. There's a natural progression. So we can do some things to move that along. This coronavirus is nothing really new. So I don't know - we don't seem to be learning the lessons. We saw this with SARS. It came out of wildlife. We know that was linked to bats. We know Ebola is linked back to bats. We know some of these new corona - the MERS coronavirus, it really looks like its origin was in bats and then got into camels.
Avian influenza, we learned years ago that if we better monitor or actually close down a lot of live bird markets, we reduce the risk of avian influenza in the United States. I think in New York, there's 20 or 30 live bird markets, just - live animal markets, just a few years ago, and I think now it's down to three or four. So once again, I think our culture's changing. There's an opportunity to reduce that risk. That's a lot like, I think, about with traffic fatalities. Some people say, oh, you shouldn't change culture. A lot of people like to drink and drive. We shouldn't really interfere with their culture of doing that. I don't agree with that. I think there's some things we can do to change - to help push along and help some cultural change to get people less - to use these live animal markets and the consumption of wildlife down. Our work with the Wuhan Institute - we've been using NIH NIAID grant funding. We've been working with the folks in Wuhan for years. We found at least 50 new coronaviruses that match up very closely related to this current one in people. It's circulating in China. When we actually tested humans, when we tested people, about 1%, a half a percent, 1% percent have antibodies. So this is going on. People have been getting these viruses for quite some time. And I think in some ways we're just lucky that it hasn't turned into an outbreak sooner.
So I just really want to finish with that because we do - as the senator said, we tend to think about the response. You know, what are we going to do? How are we going to treat these people? And I'm a firm believer we can reduce the risk of these outbreaks. We'll never eliminate all of them, of course. But wouldn't it be nice to eliminate or reduce them by 10% or 20% so the available limited resources we do have for a response could be used more effectively and have a bigger impact if we can reduce the number of these? I think the social behavioral change is great opportunity right now. There's nothing like a good disease to get people to think about what they do. But beyond that, it's really about good education and getting - and shifting people away from unhealthy practices. And I think I'll just close with that. Thank you.
LIEBERMAN: Thank you. Thanks, Billy. I'm just going to ask you a quick question. I take the - one of your big points, which is that we ought to be changing consumption habits about people who are eating either carriers or those who are likely to be infected by - that is, foodstuff. You know, I said in my opening comments, everybody says, we're moving around a lot; people are moving around a lot more than we used to - air transportation, etc. So we naturally carry infectious diseases with us. But the animals move around a lot, too. The birds move around a lot, too. The bats do as well. And is there anything we can do to stop those initial carriers of the disease? Or is that why we just have to assume we're going to be living with infectious disease outbreaks forever?
KARESH: I think that's a great question. So you know how you say in AA, you can change the things we can change and otherwise, you can accept those.
LIEBERMAN: Yeah. Yeah.
KARESH: So we were thinking about migratory birds and the spread of influenza. There's not much we can do about that. The wildlife trade, though, is purely driven by people.
LIEBERMAN: Right.
KARESH: So as you see in these markets, basically around - and certainly the case in China, much of the wildlife has been hunted out over the years. So they're importing animals. They're bringing animals from farther away. In that market in Indonesia, those bats were coming from 100 and 200 and 300 miles away, being brought by traders. So we're really moving, we're really pushing that system to feed that - whatever that demand is. In China, a lot of that trade is illegal. So they have things in place. But, you know, as we know in the U.S., illegal activities still do happen. So it's really about gearing up with law enforcement. But I was saying, once again, it's also about changing consumer desires and demand. And I think as a people - I mean, traditionally, you went to a live animal market because that was the safest place to get food because there was no refrigeration. Now we have an alternative that actually provides safe food.
LIEBERMAN: Hear, hear.
KARESH: So I think as we expand that, we can move along with people's thinking.
LIEBERMAN: OK, that's very helpful. Next is Dr. Daniel Chertow here from the National Institute of Health, but a lot of significant accomplishments along the way - Captain of the U.S. Public Health Service, head of the Emerging Pathogens Section Clinical Care, medical - Medicine Department, Clinical Center and laboratory Immunoregulation at the National Institute of Allergy and Infectious Diseases at NIH. Thanks for what NIH is doing every day and particularly now working on a response to this coronavirus. We're glad to have you here.
DANIEL CHERTOW: Well, thank you, Senator Lieberman. It's my honor to be here, and I appreciate the invitation. So I'll keep my initial remarks relatively brief. I've prepared a short statement I'd like to read to the group. So, again, I'd like to thank the commission and the Hudson Institute for the opportunity to participate in today's discussion. It's my honor to be here among such an esteemed group of organizers and discussants, including yourself, Senator Lieberman, and my co-panelists, Dr. Gerberding, Dr. Karesh, Mr. Morrison and Mr. Brown. We're here today because in early December of 2019, Chinese officials reported a cluster of pneumonia in Wuhan, China. Within weeks, a novel virus, termed the 2019 novel coronavirus, was isolated from a human, and its full genome was sequenced and reported in the medical literature in a very short interval.
This virus emerged from its natural reservoir in nature, likely bats, as Dr. Karesh has indicated, and likely passed into humans via an intermediate animal host, which has yet to be established. Regardless, once the infection in humans was established, the virus has proven to result in efficient human-to-human spread within communities, households and in the health care setting. Infections are now widespread in China, and exported cases regionally and internationally are on the rise. The most recent epidemiologic data reported from the World Health Organization on February 9 indicates that there are greater than 37,000 laboratory-confirmed cases reported with more than 8000 deaths, with the predominance in China but regionally exported and internationally exported cases to 24 countries. Rapid dissemination of information about this virus through public health authorities and in the medical literature have provided important insights into the clinical and epidemiologic features of the virus. Based upon available WHO data among laboratory-confirmed cases, approximately 15% of infected individuals develop signs and symptoms of lower respiratory tract infection consistent with pneumonia, and approximately 2% of the reported confirmed cases are - result in a lethal outcome or are fatal. Now, it's important to note that this reported case fatality is likely an overestimate, and that should be a point of discussion today, as more mild or asymptomatic cases are likely going undetected.
Among hospitalized individuals with confirmed infection, reported case fatality is higher; that's around 4% based upon recent publications. Preliminary estimates indicate that this virus is at least as transmissible as influenza, with every case infecting, on average, two or more individuals. Given these details, appropriate public health efforts to slow the spread of this virus are underway. These include travel restrictions and screenings, isolation of cases, contact tracing and quarantine of potentially exposed individuals. Preparedness at the individual level and at the institutional level, both at local health care facilities and health care systems within local, state and national levels is warranted, and it is ongoing. Those are my initial remarks, and I will cede the floor.
LIEBERMAN: Thanks, Doctor. That was great. We'll be back to you. I always ask you, Dr. Julie, how to pronounce your last name.
JULIE GERBERDING: Oh, you know, it's like the baby food.
LIEBERMAN: Gerberding.
GERBERDING: Gerberding.
LIEBERMAN: That's what I was going to say. That's exactly the same answer you gave me last time, which is unusual in Washington.
(LAUGHTER)
LIEBERMAN: Dr. Gerberding has been the director of CDC, Centers for Disease Control - and I stress today - and Prevention. She left that post, and she now has a position as executive vice president and chief patient officer, strategic communications, global public policy and population health at Merck. So she brings with her two really important elements of this, which is the work that CDC should be doing, has been doing in the role of private pharmaceutical companies in both responding to this crisis and helping us prevent the next one. Thank you for being here.
GERBERDING: Thank you. Thank you for having me and for focusing this kind of expert attention on this issue. It's a privilege to participate. I thought what I would do in my opening remarks is just remind people of how an outbreak unfolds and how the strategy has to change over time, depending on what phase of the outbreak you're in.
LIEBERMAN: Good.
GERBERDING: So if you think about what happened first - so there was a localized outbreak. And the first thing that has to happen after the emergence of this - what is presumably a zoonotic infection is the recognition and then the reporting of that outbreak. And while that seems to have happened much earlier in the course of the outbreak than it did when I was experiencing SARS at CDC, we can never be fast enough to really get that real-time understanding and that real-time diagnosis of what's going on. Once there is an outbreak, the next phase is, really, containment. And we have seen, I think, the most sophisticated and complete containment effort that has ever been invoked. I don't know, if you go back to the beginnings of quarantine, when the ships in Venice were kept in the harbor for 40 days, whether maybe that was an even more extreme case. But I think what's going on in the - in Wuhan has got to be, from a population basis, the single most massive containment effort. And then you surround that with the travel restrictions that are being implemented by countries around the world. This is definitely the best possible effort to really try to contain something at the source. The next phase is the spillover phase, and we have already seen that. There are more than 300 cases of coronavirus infection that have occurred in other parts of the world. Some of them have led to some secondary cases.
But just this week, we're beginning to see cases in people who aren't directly linked with travel in China. And as Dr. Tedros, the director general of the WHO said today, those are sparks that could ignite a fire of sustained local transmission. There's not a fire yet, but those sparks are what's really worrisome today. If you do get sustained local transmission, then obviously the strategy changes. Containment is no longer the goal; the goal is to slow down the spread and try to reduce the peak because the peak really impinges on our ability to provide care and sustain essential medical services, as well as all of the other essential services that societies need to provide for their citizens when they're under stress - so all the continuity of government, the continuity of safety and security, the continuity of food security, et cetera, et cetera. So when you move into this phase of trying to slow down, that's where the social distancing becomes important - early school closures, avoidance of mass congregations, et cetera, et cetera. The goal isn't necessarily to keep it out because it's probably too late for that, but the goal becomes, can we slow the progression, smooth the curve, reduce the overall stress on the system and, hopefully, save lives in the process of all that.
And once we see what we do every year with seasonal influenza, where we have widespread sustained transmission, you really just move into a situation where you're trying to manage individual illness and encourage people to take commonsense precautions to protect themselves. So, you know, right now we're at this kind of spillover phase of this epidemic, and we don't know what's going to happen next. We have some information, as you pointed out, about the fatality rate being much higher than we would expect with seasonal influenza, but not as high as it is with SARS or MERS. And at the same time, when people are infected and how long they remain infected is very worrisome, particularly if there does prove to be more of the asymptomatic transmission, which, by the way, does happen every year with influenza. So we really are desperately seeking the parameters that define the speed of spread and the risk of transmission at various stages of illness. And candidly, I'm worried about that.
LIEBERMAN: Thanks. I'm wondering if I can ask you just a layman's question, which is, what are the ways in which this coronavirus spread could end? Presumably, if we develop treatment, medications, that's one way. That's going to take a while in the best case. Does it play itself out? In other words, what does the science tell us about how this comes to an end? Let's assume for a moment - unfortunately, but let's assume, that we don't develop treatments, does it just keep spreading? People ask me that question. Or does it stop of its own...
GERBERDING: So that's an important question. We don't know the answer to it. With SARS, containment occurred.
LIEBERMAN: Right.
GERBERDING: After 8,000 cases, SARS was completely quenched. But SARS mainly spread from really sick people in hospitals, where you could implement all of the infection control precautions that we know would be successful and really quench the transmission. We've seen the same thing happen with most Ebola outbreaks, where once you know there is a problem, you implement the proper protection so that the sick people aren't transmitting to well people, and you can, at least temporarily, contain the problem. MERS, on the other hand, the - another coronavirus that is a very high fatality rate, about 34% percent, MERS is still being transmitted. It's coming from camels to humans. It's percolating along. And occasionally, one of these MERS patients gets admitted to the hospital, people don't recognize they're infected, and they become what we also saw in SARS, a superspreader, where they are the source of infection for health workers, for other patients and for visitors to the hospital. So incomplete containment, even in modern times where we have diagnostic tests, we haven't been able to completely contain measures. So I suspect that we can reduce a significant amount of the hospital transmission of coronavirus when the tests are widespread and we have patients in isolation or in places where there is a supply of masks and protective equipment. But, you know, the supply chain is very worrisome right now. And whether we can scale that level of protection to a number of communities that might ultimately be infected, that's a very worrisome aspect of this.
LIEBERMAN: Thank you. It's a foreboding but helpful answer. Next, we've got the honorable Tim Morrison, now a senior fellow right here at the Hudson Institute. I met him first long ago when he was a very critical and important staff member for colleagues of mine on Capitol Hill, notably my dear friend and colleague, former Senator Jon Kyl. More recently, he's been - I want to get the title correct - deputy assistant to the president, President Trump, for national security, former special assistant to the president and senior director for weapons of mass destruction and biodefense. And Tim, at our commission, we give you a good amount of credit for the promulgation by the Trump administration, not only the promulgation of a national biodefense strategy, but it's a first-rate strategy. So thank you for that.
TIM MORRISON: Thank you, Senator. I appreciate it. I think it was about a year ago I was here today to talk about that strategy. And the fact that you invited me back I think is the most gratifying thing.
LIEBERMAN: (Laughter).
MORRISON: So as you mentioned, prior to leaving the administration and when I came here to speak before you last year, I was the senior director for weapons of mass destruction. We also called it counterproliferation of biodefense. And so one of my jobs was to help the president to develop the National Biodefense Strategy. And I've been a staffer long enough to know never to try to take any credit. It was the boss's doing. And really, what I think the president was looking to accomplish was to have a system where he could have accountability, so building on the good work that had been done by the Obama administration and the Bush 43 administration. I think the president originally if I could just step back one further - in the FY '17 National Defense Authorization Act, the Congress actually asked the administration, talk to us about how you handle biodefense. And they principally chartered HHS, the USDA and DOD. And in answering that and then taking what the answer was going to be to the president, I think the president said, well, this isn't enough, and I want to know who's actually in charge of biodefense. And this is something the president had written about as far back as the year 2000, again, basic staff work. Working for the other senator from Arizona, as we like to call Senator Kyl...
LIEBERMAN: (Laughter).
MORRISON: ...We stepped back and we found that, really, every federal department is involved in biodefense from DHS to DOT, obviously USDA, interior. Biodefense touches every part of every executive department and agency. And it's also throughout every element and every facet of the intelligence community. And so in terms of trying to wrap our arms around that and trying to answer the mail for the president who's accountable, who's in charge, the biodefense strategy, NSPM 14 was born, which set up a process, again, building on, I think, some very solid work that was done by the two previous administrations to allow the president to wrap his arms around what the priorities are in each of the departments and agencies that have a role in biodefense. How do you put that together in terms of a cogent plan and a cogent budget that can be then sent over to Capitol Hill, as was done today for the FY '21 budget, where the Hill will then chop it up into 13 different budgets through the appropriations process but still try to keep it in terms of some sort of place where you draw the line because budgets are limited. Even when the budget today was about $4 trillion dollars, budgets are limited, and there's always priorities that're going to fall above the line and below the line. How do you package that up and try to put together one, overall picture where the president can then look across the interagency - and we have a video of an interagency meeting, too, but it's definitely not suitable for an open forum like this...
(LAUGHTER)
MORRISON: ...If you want to talk about how the sausage is made, fewer bats in our process. But that is an annual process, the NSPM 14 process, to pull all those budgets together, all those different programs together from all the executive agencies and, in fact, the intelligence community, and try to put together under one, unified set of priorities. And then the president knows who to look to. And I think you saw that play out when he announced his task force for coronavirus - was he immediately went to Secretary Azar, and he immediately went to the national security adviser because that's what NSPM 14 told him. That's the process he set in place. And so the administration has had a number of opportunities to talk - to show how this process works because since it came forward - first of all, there was the sausage-making of the strategy. The administration promulgated the global health security strategy. The administration promulgated the influenza executive order to streamline vaccine production.
One of the most amazing things to me in helping to work through that process was just how much of our vaccine production is still tied to eggs, which when you think about where we are in the 21st century and the, you know, the fact that every one of us has a has a phone - hopefully nobody has a Huawei phone - but every one of us has a phone with more computing power than the Apollo program, and yet we're still making our vaccines with eggs, trying to - that was one of the goals of the influenza executive order was, how can we change that process to make a vaccine production supply chain that's more nimble and responsive to what we actually see? And then, of course, Ebola - and the Obama administration before the 2014 West Africa outbreak did a lot of significant work. A lot of those lessons were wound up - we baked them into the NSPM 14 process. But getting our arms around the Ebola in the Congo, the most challenging - feel free to disagree with what you saw - but in the Congo, we encountered the most unstable security situation for an epidemic outbreak, I think, that we've ever seen. You found an outbreak in a part of the country that simply did not consider itself bound to that government. In fact, there were concerns about the fidelity of their election in the middle of the outbreak just to really make sure that the population didn't trust the government. These were the kinds of things we were dealing with.
But the NSPM 14 process, the biodefense strategy, I think, wound up proving itself out to help the interagency, help the president with the options that he would need to help marshal all the resources of the United States government, the WHO and allies, to help get that outbreak under control. And so that was the process. Those were the lessons that we learned. And I think that's a process that's largely working today. There have been no significant calls for the kind of Ebola czar that was needed in 2014. I know people continue to talk about it. But I think, by and large - and maybe it's just a function of who I talk to - I think, by and large, people believe that the process that was set up is largely working. The gaps that people have previously feared when these were more - pardon the term - more novel episodes for the government to handle I think aren't there today because of the lessons that have been learned before. And really, what we wind up finding is the biggest gap where we're dealing with is the information we get out of China, and can we trust it? Are we getting a fulsome picture? But for the purposes of the interagency, I think the process that the president set up is largely working. And hopefully, that continues to play out as the United States government gets its arms around, how do we respond to this particular outbreak?
LIEBERMAN: Right. Thank you. Eric Brown is also a senior fellow here at the institute - Hudson Institute and is an expert on China and Chinese government and policy, so we're grateful to have you bring that important element to this discussion.
ERIC BROWN: Let me caveat everything that I'm going to say by saying I have no public health background. I'm a science junkie, so I'm very much here and grateful to be able to hear what all of you have to say about this. I mean, most American citizens, I think, have been hungering for some rational, scientific explanation about what we're looking at in the coronavirus outbreak. I think the opacity and the lack of fulsome information from China itself has contributed to a lot of conspiracy theories, fringe theories, among other things and general fear. And I should say that that's general fear not just in the United States, but in China itself and in the countries that surround it. There is a general - I think, a general sense that that the PRC numbers and what the PRC says - what the Chinese Communist Party says - about the outbreak is not credible, that it's, in fact, politically skewed by what the party itself wants both its subjects and the wider world to hear.
And on that account, I want to say that I don't think that the party's response to the crisis is very surprising. I mean, at first, last year, officials in Wuhan - party officials, at the direction of Beijing - had scrambled to cover up the epidemic. And now, people from all walks of life are being threatened and punished by the party state for not reporting on the pandemic or complying with other party dictates. Neighbor is being turned against neighbor - you can visit Weibo and social media to see evidence of this - while tens of millions of Chinese are under lockdown. And the central government is saying it has everything under control. And yet, there is a persistent question, is that, in fact, the case? And are these draconian measures, in fact, necessary? I'll take your word for it, but from my perspective, I highly doubt that a city like Los Angeles would countenance being locked down the way the citizens of Wuhan have been locked down. All this, in fact, fits a pattern with how the Communist Party has responded to comparable crises in the past, for instance, the HIV-tainted blood supply that blossomed into a full AIDS epidemic in the 1990s, the SARS epidemic of 2003, as well as other issues and crises surrounded - contaminated - surrounding contaminated food supplies.
First, the CCP has a habit of denying that this is happening. Then the party spins and lies about the extent of it or gives bad information. Then it responds with draconian measures and underplays the extent to which the crisis has happened and the damage it has caused. It's - I'll add that it is, in fact, the party's M.O., not just when it comes to public health crises, but in all instances where it faces political embarrassment and its competence and the power of its claims to power are called into question. Look, for instance, at Beijing's bid to cover up the mass atrocities and gulags in Xinjiang, which is something that we've studied very closely here at the institute. I was very glad to see Secretary Pompeo and the administration, as well as leaders in Congress, call for a robust effort to mobilize money and U.S. health expertise to help China arrest the epidemic there. I would argue that, objectively speaking, the U.S. is the most pro-China country and has done more for China than any other foreign nation over the last 150 years. That's a political statement, but it's borne out by anybody who studies the history.
I do worry, however, that even this sign of goodwill is not going to change much about the CCP's behavior. And we know how the CCP has responded to other crises, particularly in the last 10 years and particularly since the rise of Xi Jinping, and it has led not to greater liberalization or greater accountability of party officials but rather to the opposite. Instead, what we see today is the CCP's propaganda apparatus or narrative spinners has kicked into overdrive, and it is relying more and more on nationalism and paranoia to divert people's attentions from the party's own failings at home. It is attributing the regime's problems indeed to responding to - in responding to the crisis to foreign machinations. U.S. health officials have not yet been allowed to go, I think, en masse. And without getting a proper assessment of what's happening, we can't provide our own expertise. So this is the PRC politicizing the problem.
And yet the PRC's ambassador to the U.S., just the other day, said that the U.S. is politicizing the virus outbreak. I find this to be particularly rich since it is, in fact, the CCP state that has politicized the very international health bodies that are supposed to fight these pandemics and keep them contained. Taiwan, for instance, is a frontline nation in responding to the crisis, but the PRC's successful efforts to exclude Taiwan from participation in the World Health Organization is putting the party's political considerations above the health of ordinary Taiwanese and, in fact, I think every country in the world that Taiwan is connected to. Taiwan is a vital frontline state in stopping the spread of this epidemic, and it has expertise, indeed, that it could offer to the Chinese mainland in the interim. I want to say that I think the social and cultural changes to wet markets - China has shown a tremendous capacity for innovation in social and cultural affairs. These wet markets have been around for hundreds of years, thousands of years, even. And I don't see why the Chinese people, with a proper education campaign, can't modernize their practices there and hopefully improve food security and the food supply to create alternatives.
The Chinese Communist Party, however, has been around since - in power, at least, since it fell - China fell to it in 1949. It's going to be a lot harder to change that. The kind of bad information that we get out of China, not just about public health crises, but about economic and military issues, among other things - this is baked into the Communist Party system. Why? Because the Communist Party is, unlike our system - which is, yes, we believe that people can govern themselves best if they are free, but we also fundamentally believe in the fallibility of human nature. And for that reason, we build up a system of checks and balances, and we encourage cross-checking and debate and lots of disagreement in the public realm. And this is the fastest way, I think, to getting a proper assessment of what's actually happening, and this has add-on benefits for governance writ large. The PRC party state is founded on the theory of dialectical materialism, not skeptical materialism. It believes - the party believes that it and it alone has the right to rule China.
And therefore, it has a political interest in preserving the myth that its decisions are infallible, that in all instances, including political public health crises like the current one, its decisions are correct. In all instances, they must be correct. What this means in practice is that the party needs to have total control of the information that comes into the country and that goes out of the country. And it's precisely this system that is producing the skewed information that we're getting out of China, and it has implications for China's governance. And with an issue like this, an epidemic that has become a pandemic, it has implications for every other country in the world. And I think that the responses that you're seeing from the U.S., from most of China's neighbors, is a sign that in matters in life and death, they're not willing to rely on the party's judgment much longer. And this is going to have implications for, I think, years to come, even if the coronavirus that we're tackling right now goes away this season. If the sun comes out and burns it up, that would be wonderful. But people don't trust what the CCP is telling them. And I'll leave it at that for now. Thank you.
LIEBERMAN: OK. Thanks, Mr. Brown. That was a straight talk, as my buddy, the other senator from Arizona, used to say.
BROWN: That's him.
LIEBERMAN: And I'd say two things. One is that - and it may be happening in this case. It - even autocratic, centralized governments are sensitive to public opinion if public opinion is so aroused that it may, in some sense, either, one, disrupt the stability of the country or, two, threaten the continuance of the autocratic government. And in recent times, we have seen the Chinese people, to be specific, be very upset, mobilized on the question of environmental pollution - particularly air pollution, but others as well. And the government responded autocratically, much quicker than the American Congress and president would respond 'cause of the nature of our process and did some very affirmative things to reduce sources of air pollution. It's obviously not perfect. So it may be, to have an optimistic view of this, that the government will feel a necessity for its own credibility and to avoid domestic instability and worse, to take action some of the ways they can.
And the other thing - and from our point of view, and I want to just, before I have some questions from the audience, ask others to comment from their perspective. So we - I think we in the United States have to ask ourselves, at this moment in the history of our relations with China, which have been contentious in recent years, although a little bit calmer right now - none - and because of all of our difference in values, approach to government that you talked about in some ways, nonetheless, there are, what I'd call both moral and practical reasons why we have to try very hard to engage with the Chinese government and try to be constructive in response to this kind of public health crisis. The moral one is, of course, these are people in China. They're our fellow human beings. They're being infected and dying at an alarming rate. So to the extent that we can help the Chinese government and people stop this, that's, I think, a moral imperative, and it's one that's traditionally been accepted by America in a lot of other natural disaster cases. And the second is what you talk about, which is, you know, it is, as Mr. Disney told us a long time ago, a very small world. And our inner connections, the American people with China - whatever our - the nature of our political relations economically and tourism - just remarkably intense. It's impossible to separate.
I saw a number recently - not just to America, but 150 million visits by Chinese people outside of China every year. That's quite something. And so I guess the question is, in a situation that can be difficult - there's national pride; there's political authority on the line - and whether any of you want to comment on the extent to which in your areas of expertise - is something constructive is happening with China - either Chinese government or independent groups there - or what can happen? What should happen? Dr. Gerberding, I wonder about you, both in terms of your previous life at the CDC, but also the pharmaceutical sector.
GERBERDING: Yeah. So I have a memory in my mind of my time at CDC that has really colored how I'm thinking about sort of this tension between autocratic government, and humanitarianism, and the moral and social responsibility that we have to do the right thing when people are suffering the way these people are suffering. My predecessor at CDC, Dr. Jeff Copeland, established a relationship with the China CDC when it was very small and nascent. And I tried really hard to build on that. So we established a memorandum of understanding between the U.S. CDC and the China CDC. And almost every year, the China CDC would bring its most senior leaders to Atlanta, and we would have as scientist-to-scientist colloquium. And then in the opposite year, I brought all of my leaders to China and sat down at their CDC. And after the concern about avian influenza emerged, I went to China with the leaders. We sat in the new China CDC Emergency Operations Center. We linked to the operation centers in every province. We met with the scientists. Our flu expert had a very interesting scientific exchange about flu surveillance and so on, so forth. And then we went in front of the building and had our picture made, all of the CDC leaders. And they flew the American flag and the Chinese flag.
And in that moment, I felt like the front line of global health security was sitting in that tableau because if we can't figure out how to cooperate in the context of a global health emergency, everyone will suffer. And I just keep coming back to that memory as I think about, you know, what should I as a leader at Merck do? What should the industry do? What should we as Americans be doing? You know, right now, we have several thousand employees in China. We're very concerned about our Chinese colleagues in our company. But we're - I, as the chief patient officer, am especially concerned about the patients that we have in clinical trials for things like cancer because these patients need their medicines. And if we can't figure out a way how to sustain their therapy, they will die not from a coronavirus, but they will die because they can't get the medicines they need in the health system that's overwhelmed with - worried well, as well as the affected people. So I think we have to really kind of back up from our political lens alone and broaden the aperture to consider in even more important humanitarian terms of engagement.
LIEBERMAN: OK. That's a great memory. If I heard you right, Merck is doing clinical trials on cancer medications in China.
GERBERDING: These are not clinical trials for coronavirus.
LIEBERMAN: No, understood.
GERBERDING: These are cancer patients.
LIEBERMAN: Yeah. So that's fascinating and, again, shows us what a small world it is 'cause I bet most people in the U.S. would be surprised to hear that you're doing clinical trials in China, but why not? If you - if it works...
GERBERDING: People are suffering.
LIEBERMAN: People are suffering, and it'll be - the impact will be global if whatever you're trying will work. Dr. Chertow from NIH, how about connections and partnerships with your Chinese colleagues?
CHERTOW: Yeah, I guess I would respond to the general part of the conversation by echoing what Dr. Gerberding said, which is sort of simply put that, you know, we need each other. I mean, it is a very interconnected world. And microbes don't respect international boundaries. We know that. And the example is, you know, playing out again. The question of, you know, what has been done well so far and what might have been done, perhaps a little bit better - you know, as we said previously, in a remarkably short interval, the recognition of a new, severe pneumonia clinical syndrome; the identification of an electron micrograph of the organism in a very short period of time; the full genome sequencing; the relationship of that sequencing to known bat coronaviruses that have been pulled out of bats to give us some insight into where this pathogen may have - may be hiding in nature; the relatively rapid reporting of clinical and epidemiologic information that has been published in major medical journals, including The New England Journal of Medicine and The Lancet with active, ongoing websites that are being continually updated where relevant, epidemiologic and clinical information about this disease that are really important for decision makers are being shared - all of those things are really, really excellent.
I think what, you know, has been stated and is quite obvious is that, you know, the United States, between the Centers for Disease Control and Prevention and certainly, you know, folks at the National Institutes of Health, we have enormous capacity and capability, global expertise with disease prevention and control. And we certainly would like our experts to be present and to be part of what's going on in the ground to answer some really important, fundamental questions - one of which is, you know, what is the denominator? You know, how I mentioned this 2% case fatality rate. Well, is it 2%? That may seem low compared to SARS 10% or MERS, you know, 34%. But compared to seasonal influenza, 1 in a thousand to 1 in 10,000 - compared to the 1918 pandemic, you know, 1% to 2% case fatality rate, it's pretty high. But is that the true case fatality rate? What's the denominator? That's a really important question for our folks. And then the other question that Dr. Gerberding mentioned as it relates to, what is the likelihood that our control - prevention and control practice are going to work? Is there asymptomatic shedding?
You know, we mentioned influenza. Influenza has about a two-to-three-day incubation period, where you're exposed before you begin - before you begin to have a manifestation of illness. But - and within that two-to-three-day period, there's about a 24-hour period where you have no symptoms and we know that you're shedding the virus. Well, what does that look like for this virus? It has really, really important implications for policy planning to say, what of the different interventions that we're going to make are going to control this outbreak? And as you asked the question about, you know, NIH. Obviously, our mission relates to biomedical research, which has to do with, you know, vaccines and potential therapeutics, you know, shared efforts of looking at, you know, potential promising antivirals, you know, in coordination. That has to do with the design of the clinical trials to look at safety and efficacy. Rather than having duplicative efforts between the United States and China, those efforts should be, I would suggest, coordinated.
LIEBERMAN: Excellent. We have questions from - you want to...
KARESH: I have just one thing.
LIEBERMAN: I like you, you know.
KARESH: (Laughter).
(CROSSTALK)
LIEBERMAN: So yes.
KARESH: OK. I just was just following that line of thinking because there's the political side, so I'm on board with you there, but we tend to think of this as so much as government, government, when, in fact, the beautiful thing in the U.S. is most of us actually aren't in government. And the same is true in China. And there is a lot of interaction. You know, there's some interesting programs. Like, USAID has been supporting U.S. scientists and health care workers to build collaborations. DTRA has a biological engagement program about to (ph) collaborate. NIA does a great one. NIH - we've been working in China with NIH supporting AID. And those relationships are pretty amazing over the decades.
LIEBERMAN: And also with non-governmental entities...
KARESH: Yes.
LIEBERMAN: ...Educational...
KARESH: Yeah.
LIEBERMAN: ...Public health.
KARESH: You know, in China, it's always hard to decide what's really not government...
LIEBERMAN: Yeah.
KARESH: ...Because their system, but...
LIEBERMAN: ...Or - but at least it's not officially governmental.
KARESH: Exactly. So we don't have to discuss with the State Department, is it OK to make a phone call?
LIEBERMAN: Right.
KARESH: So we pick up the phone, and we talk to them. So in this case, we've been learning a lot from these viruses and getting emails from colleagues there. So there's some - and built into our system, we have some - I don't know if you should call them workarounds, but they're like alternative pathways. And the private sector's doing that. So again, in some ways, that's encouraging. And we see in the Chinese society amongst the people, they're also interested in that. I am - the alternative to not being engaged is just to paddle around at night in your canoe and wait for something to jump over the transom and try and react.
LIEBERMAN: Right.
KARESH: So we need some ways...
LIEBERMAN: Yeah, while people on the other side of the transom are dying.
KARESH: Yeah.
LIEBERMAN: Yeah.
KARESH: Oh, yeah. And had that - this disease broken out in Indonesia in that market, I don't know if they would have responded half with the same capabilities as China. So there's something - you know, there's a complex story that's going on. But, I mean, I'm certainly on board with you about things that could improve there.
LIEBERMAN: OK. There - that leads me to ask you some questions asked by the audience, and two of them go together. One is about Indonesia. The first is, notwithstanding reports of wildlife trade and consumption in Southeast Asia and China, the NCOV originates from Wuhan. What's the defining difference that results in this outbreak in China and not one of the other Southeast Asian countries? And if I may, I'll add the second question, which is related. Regarding the video clip showing wildlife sales in the Indonesian markets, Indonesia has actually not reported a single novel coronavirus case. Can you share an assessment of whether it is a case of underreporting or insufficient capabilities or perhaps a natural resistance against such a disease spreading in Indonesia?
KARESH: I - well, you can help me on this. My - I would say all of the above. But I would - with Indonesia, I don't - if it's under - being underreported, it's because it's not being detected or diagnosed. And I think they don't have the same rapid capabilities that we see in other countries, including China. These spillover events, like I was saying, it's, like, 1% of the rural population of China - 1% would be 5, 10 million people have antibodies to these coronaviruses. And it hasn't turned in - none of those have turned into a pandemic or...
LIEBERMAN: Right.
KARESH: ...You know, a thing (ph). So I think this is happening all of the time. It's probably happening in Indonesia, and Thailand, and Malaysia and Myanmar and throughout the region and Vietnam. Most of them are dead ends. They don't go very far. It's just, everyone wants - one, you know - one became HIV/AIDS. It hasn't gone away yet. One became SARS. Most of them - they're happening all the time. Most of them are dead ends.
LIEBERMAN: Yeah.
KARESH: And luckily for us, they don't go anywhere.
LIEBERMAN: So that's a good point. So we're all, including me, learning about something called the coronavirus. But those of you who are active in the field, I've learned, know that there are a lot of coronaviruses and they've been around for a while. This one just happens to be taking off in a way that's quite harmful.
KARESH: Yeah. We have two that cause the common cold it looks like entered the human population...
CHERTOW: Four.
GERBERDING: Four.
KARESH: ...Well...
GERBERDING: Four.
KARESH: ...Two that look like it...
CHERTOW: Four.
KARESH: ...Came from bats about 100 or 200 years ago, only in the 1700s entered humans.
LIEBERMAN: So dare I ask, is it possible that we will contain the current pandemic - in some ways, bring it to an end - and yet the virus that has led to it will stay around in the human family for quite a while?
GERBERDING: I have to admit, when SARS emerged - and the wet markets weren't any better than they are now, so it seemed almost impossible to me it wouldn't be back.
LIEBERMAN: Yeah.
GERBERDING: And, you know, we haven't seen natural recurrence of SARS except for those patient who had that related SARS coronavirus. But we really didn't see SARS again - very mysterious. It tells you we have a lot to learn. There's also a conversation about seasonality. The coronaviruses that we all get - about a third of us every year with the common cold - are winter viruses. They go away in the summertime in the northern climates. In the more tropical areas, there's less seasonality, so we have to remember not to be falsely reassured by this just because many people living in colder temperatures aren't plagued with respiratory viruses when it's warm outside. Lots of people live south of the equator and lots of people would continue to be at risk for non-seasonal infections - so just much more to learn. And I really would hesitate to look in the crystal ball on this one.
LIEBERMAN: Yeah. Here's a question that probably a lot of people across the country are asking themselves that has been asked from the audience. Exactly how does one determine whether a patient has the Wuhan coronavirus? Are false positives common? Dr. Chertow, you want to try that?
CHERTOW: Sure. So you know, I think up front, there is a surveillance or a case-finding definition, which simply put is, you know, sort of two features combined. So it's an individual that has evidence of a respiratory illness - fever, cough, breathing quickly, shortness of breath - plus an epidemiologic risk factor. And right now, that epidemiologic risk factor is either traveled to a region where there are cases within a 14-day interval, which is on the long end of the incubation period for the virus - so a clinical syndrome, plus epidemiologic risk factor, which includes either travel to an affected region within 14 days or contact with a suspected or confirmed case - so a clinical feature and an epidemiologic risk factor. Those individuals then are flagged, and they're tested.
And the testing is done predominantly on respiratory secretions, both from the upper and the lower respiratory tract. And there's a test that is a very sensitive and specific test. It's a molecular test that was established at the CDC and now is being pushed out to state health departments. That, as I say, is quite sensitive. If it's positive, that means that you've got it. If it's negative, you have to be careful in the interpretation of the test because even though the test is quite accurate, depending upon where you are in the course of illness, you may or may not be shedding from the upper versus lower respiratory tract, which is why there is a recommendation for testing of multiple specimens and perhaps testing repeatedly over the course of the clinical illness.
LIEBERMAN: You want to add anything, Dr. Gerberding?
GERBERDING: No. I think I'd like to just go back to the Indonesia question, though, because in medical school, I learned that there was no fever if there's no thermometer.
: (LAUGHTER)
GERBERDING: And I think that we have to be, you know, mindful of the fact that the test is not universally available, so we could be missing cases.
LIEBERMAN: Yeah. Let me ask you a question, then, and at the other end of your experience, which is, what can the government best do to be supportive of the pharmaceutical industry in bringing about, if it's possible, a broad-spectrum antiviral medication so we're ready the next time this happens? It's hard for the pharmaceutical industry, I know, because you're not sure when it's going to happen, so it's not a certain market - a clear market like a continuing illness that affects a lot of people.
GERBERDING: So a little context here because the - you know, the government has been working on this since at least the Bush administration and probably before that, and that's where the investment in BARDA, the biomedical - you know, the advanced research development capability that allows our government to invest in biotech and pharmaceutical companies and device companies to work on countermeasures in advance of the appearance of a particular problem, building vaccines, antivirals, et cetera, et cetera. And then there's the Strategic National Stockpile, which is our hidden-in-plain-sight warehouse of all kinds of durable medical goods and medicines. So the problem is, is that the list of what might happen, of the things we even know about, is very, very long. And then there are the things that haven't appeared yet that - you know, how can we make a countermeasure for something we haven't recognized? So increasingly, investments are being made in platforms. I'm sure that there is a lot of energy right now around creating a coronavirus platform that would allow the rapid introduction of the specific parts of a new coronavirus that would be most likely to be immunogenic to kind of speed up that process. So that's one really important thing that the government is already doing. And we can sustain the funding of that and even do more, I think.
The second thing is, the government could support CEPI, and I hope people here have heard of CEPI. It's the Coalition for Epidemic Preparedness Innovation. It's a private-public partnership that includes governments, the Gates Foundation and the Wellcome Trust, lots of partners that have pooled their money and are able to very rapidly respond in a crisis. Already, they've put three grants out for coronavirus countermeasures. But in addition, their goal is, for the things that we know could cause serious outbreaks or pandemics, to work on the vaccines and the countermeasures up through Phase 2b even before they have emerged. So it's - again, it's an accelerant trying to engage small companies and large companies in putting more effort into these emerging threats. And that would include, we hope, in the future, antibiotic resistance, which, of course, will be a major bottleneck if we actually do end up with a very large outbreak and have sick people in hospital with complicating bacterial infections. So I think the government needs to step away from our current mindset about the nature of this threat and really think about it in the same frame that we think about other issues of national defense. We are not making an investment commensurate with the degree of threat - and not just threat to human lives, but threat to national security and threat to lives and limb. So our mindset is, how can we do something? But it isn't really, how do we take this off the table? And, you know, we always use the DOD analogies, but what we're investing to protect our nation against these threats is really very small compared to what we spend on other elements of national security.
LIEBERMAN: That is a really important point, and unfortunately, because of the coronavirus pandemic, we're seeing some of the costs. I mean, the markets have been gyrating. Businesses are dropping. You can see just every day, there's another report of the impact on the Chinese economy of this coronavirus outbreak and, therefore, the impact of the troubles in the Chinese economy on the economy of the world, including our own, because we're so interconnected, let alone the fact that a lot of American-based businesses are not able to do business or decide not to do business in China now. So, I mean, I don't know if anybody's even tried to calculate, but my guess is that the loss in dollars from the coronavirus globally is going to come in in the hundreds of billions. And therefore, it's worth investing some now to try to avoid it. Tim, I'm going to give you an opportunity now that you're outside of government (laughter) to say what you think, based on your experience here, are the one or two most important things the federal government could do, both an immediate response to this pandemic but also to get ready for the next one, which will surely come.
MORRISON: So I'll just go back to the biodefense strategy because I think that is a process that is still new, that the administration built upon what other administrations had tried to do and improved it. It's the old Newton line that we stand on the shoulders of giants so we can see farther. I think they built on the progress that earlier administrations made. And so continuing to implement it, the - if there's one thing that I came away from the National Security Council with, it was the line from John Bolton that the process is your protection. So stick with the process, and that's what gets things done. It's that long, slow grind that is the work of government. You know, the - I've had a number of folks call me up and say, why is the president being so easy on the Chinese? Why does he keep saying all these nice things about Xi Jinping? And, you know, to me, you know, sort of the Donald Trump you see on TV is the Donald Trump, you know, behind the scenes as well.
He's just one guy. And I think the president is engaged in a sort of a good cop, bad cop here. I think he is trying to encourage the Chinese to resist some of the worst tendencies of insularity and opacity of the Chinese Communist Party. And he's leaving it to the CDCs and the NIHs and other organizations to be the bad cop. I think he's doing his best to try to encourage Xi to be as open as possible now. From time to time - and I didn't see the full interview. I only saw the press clip. From time to time, some of the other government officials - Secretary Ross - say things that could be hopefully taken out of context. But I think that's what the president is trying to do, is try to encourage the Chinese to be as open as possible because that's what's going to allow the professionals to get in there and get this thing solved, if there is a solve - if there is a cure.
LIEBERMAN: So that's an important point that I say, respectfully, that as I've observed President Trump, he's capable of being both the good cop and the bad cop...
MORRISON: Sometimes at the same time.
LIEBERMAN: ...At the same time or in the (laughter) same day. But - so we all understand that the tensions in the bilateral relationship with China. But also, I think - I hope people appreciate how important it is to try to - to use a familiar word, but I can't think of a better one - manage the relationship in a way that it doesn't break into open conflict because we are so tied together, and it is, after all, a small world that we inhabit. So I, for one, was encouraged when I heard that President Trump and President Xi had a hourlong conversation, much of which was about the coronavirus and how to better deal with it. And I don't - I think I have enough of a sense of President Trump to know that that doesn't end his concerns about every other aspect of Chinese policy, trade or otherwise. It bothers him. But I mean, I think this is a moment - just think of ourselves in terms of our neighbors and friends. When they have a problem - well, let's think of ourselves when we have a problem (laughter) or somebody in our family is sick, and one of our friends or neighbors - sometimes it's surprising who will do it - offers to be of help to us. We never forget that. And that may just be the case in relations between great nations like China and the U.S. I'm not as naive as that sounds.
(LAUGHTER)
LIEBERMAN: But I am as hopeful as that sounds. So we've come to 3:31. We're a minute over when we said we'd conclude this. I think it's been extremely valuable to me. On behalf of the commission, I thank all those who participated in the discussion - thank you - who came out. And we're going to think a lot about what you all said and see how we can take this forward in a way that's constructive. Thank you very much. Thank you, all.
(APPLAUSE)